By
Liz Highleyman
 Treatment
with pegylated interferon
plus ribavirin can cause difficult side effects and cures
only about half of people with chronic hepatitis C. Furthermore,
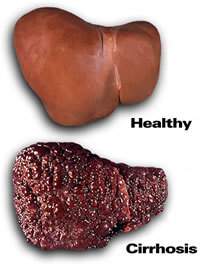
HCV leads to advanced liver disease such as cirrhosis
(replacement of functional liver cells with scar tissue) or
hepatocellular carcinoma (a type of liver cancer) in only a
minority of patients. Therefore, clinicians attempt to wait
long enough to be sure an individual is progressing and truly
needs treatment, while not waiting too long, since interferon
does not work as well and side effects can be worse in people
with severe disease.
Treatment
with pegylated interferon
plus ribavirin can cause difficult side effects and cures
only about half of people with chronic hepatitis C. Furthermore,
HCV leads to advanced liver disease such as cirrhosis
(replacement of functional liver cells with scar tissue) or
hepatocellular carcinoma (a type of liver cancer) in only a
minority of patients. Therefore, clinicians attempt to wait
long enough to be sure an individual is progressing and truly
needs treatment, while not waiting too long, since interferon
does not work as well and side effects can be worse in people
with severe disease.
Experts
have debated the best time to start treatment for people with
advanced liver disease. Interferon and ribavirin are more likely
to cause adverse events in people with cirrhosis, but these
are also the patients who stand to benefit most if successful
therapy can halt or slow disease progression.
Compensated
cirrhosis means the liver is heavily scarred but can still carry
out most if its vital functions. Decompensated cirrhosis means
the liver is no longer working properly to filter blood, leading
to conditions such as portal hypertension, bleeding varicose
veins in the esophagus, ascites (abdominal fluid build-up),
and hepatic encephalopathy (neurocognitive impairment).
Sammy Saab and colleagues sought to determine the most cost-effective
timing for pegylated interferon plus ribavirin treatment (48
weeks) in patients with advanced liver disease related to genotype
1 HCV infection -- the most difficult type to treat.
The study included about 4000 participants followed over 17
years. The investigators used a Markov mathematical model to
compare treatment 4 treatment strategies, with approximately
equal numbers of patients in each group:
|
1
|
No
treatment; |
|
2
|
Antiviral
therapy for patients with compensated cirrhosis; |
|
3
|
Antiviral
therapy for patients with decompensated cirrhosis; |
|
4
|
Antiviral
therapy for patients with progressive fibrosis due to recurrent
HCV post-transplantation. |
They
looked at outcomes including total cost per patient, number
of quality-adjusted life years (QALYs) saved, cost per QALY
saved, number of deaths, number of cases of hepatocellular carcinoma,
and number of liver transplants required.
Results
 |
 All
3 treatment strategies were cost-saving compared with no
therapy, but treating patients with compensated cirrhosis
was much more cost-effective and greatly improved survival: All
3 treatment strategies were cost-saving compared with no
therapy, but treating patients with compensated cirrhosis
was much more cost-effective and greatly improved survival: |
| |
 |
Treatment
during compensated cirrhosis: increased QALYs by 0.950
and saved $55,314 compared with no treatment. |
 |
Treatment
during decompensated cirrhosis: increased QALYs by
0.044 and saved $5511. |
 |
Treatment
during HCV recurrence after transplantation: increased
QALYs by 0.061 and saved $3223. |
|
 |
Compared
with no treatment, antiviral therapy for patients with compensated
cirrhosis resulted in: |
| |
 |
119
fewer deaths; |
 |
54
fewer cases of hepatocellular carcinoma; |
 |
66
fewer liver transplants. |
|
In
conclusion, the study authors wrote, "the treatment of
patients with compensated cirrhosis was found to be the most
cost-effective strategy and resulted in improved survival and
decreased cost in comparison with all other strategies."
"This study provides pharmacoeconomic evidence in support
of treating HCV in patients with compensated cirrhosis before
progression to more advanced liver disease," they added.
In an accompanying editorial, hepatology experts Angel Rubin
and Marina Berenguer from Valencia, Spain, offered the caveat
that models such as this do not take into account all the many
variables that can affect disease progression and treatment
response, recommending that "Physicians must decide whether
the most cost-effective approach is the most appropriate one
in each individual."
Investigator affiliations: Departments of Medicine, University
of California at Los Angeles, Los Angeles, CA; Department of
Surgery, University of California at Los Angeles, Los Angeles,
CA; Harbor-UCLA Medical Center, Torrance, CA; Huntington Medical
Research Institutes, Pasadena, CA.
7/2/10
References
S
Saab, DR Hunt, MA Stone, and others. Timing of hepatitis C antiviral
therapy in patients with advanced liver disease: a decision
analysis model. Liver Transplantation 16(6): 748-759
(Abstract).
June 2010.
A
Rubin and M Berenguer. An economic analysis of antiviral therapy
in patients with advanced hepatitis C virus disease: still not
there! (Editorial). Liver Transplantation 16(6): 697-700.
June 2010.
Other
source
Wiley-Blackwell.
Antiviral therapy during compensated cirrhosis most cost-effective
approach. Media advisory. May 27, 2010.
